Contents
Pain = unpleasant sensory and emotional experience with physical, psychological, spiritual and social aspects.
Assessment of pain
It is important to remember that pain is a symptom and not a diagnosis. The key to successful treatment is accurate diagnosis. This can be achieved by good history taking.
S Site
O Onset
C Character
R Radiation
A Associated features
T Timing
E Exacerbating and relieving factors
S Severity
Causes of pain in palliative care
- Effect of underlying pathology e.g. lung cancer
- Result of treatment e.g. neuropathy from chemotherapy
- Unrelated e.g. DVT/pressure sores
Treatment of pain in palliative care
The principles of pain relief in palliative care are:
- By the clock (regular)
- By the mouth
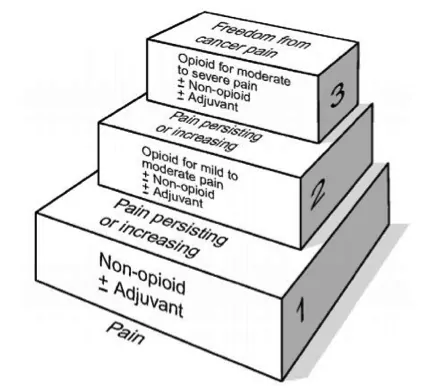
- By the ladder (use the analgesia ladder)
- Non-opioid e.g. paracetamol
- Mild opioid e.g. Codeine and adjuvant e.g. ibuprofen
- Strong opioid e.g morphine
Factors to consider when prescribing analgesia:
- Renal/liver function
- Route of administration
- Severity of pain
- Current analgesia
- Other symptoms e.g. nausea/vomiting
Morphine or Diamorphine (depending on local guidelines) are the mainstay of analgesia for severe pain in palliative patients. Initial treatment should involve a short acting opioid e.g. oramorph or Subcutaneous morphine/diamorphine if the oral route is unavailable. Once the amount to control pain in 24 hrs is known, this amount can be converted to slow release morphine e.g. Zomorph/MST via oral route or Morphine/Diamoprhine via a syringe driver. A syringe driver/pump is a continuous infusion device where the medication (or combination of medications) are released over 24hrs.
Opiates e.g. codeine/morphine commonly cause nausea and constipation. Therefore it is good practice to prescribe an antiemetic and laxative when prescribing these medications.
Breakthrough anaglesia
Breakthrough analgesia is used to treat the pain suffered despite regular analgesia. Every patient prescribed regular analgesia should have “back-up” PRN medications written on their prescription chart if they have further pain. This is normally the next step on the analgesic ladder. E.g. if the patient is on regular paracetamol, it is good practice to prescribe PRN codeine or ibuprofen (if stable renal function). If the patient is on morphine/diamorphine, 1/6 of the total daily dose should be prescribed for breakthrough pain 2-4 hourly on the PRN section of the drug chart. This should be reviewed every 24hours and the amount of breakthrough analgesia added to the regular prescription.