
Overview
De Quervain’s tenosynovitis is an overuse injury of the wrist, affecting the dorsal extensor compartment (sometimes called compartment 1) tendons – extensor pollicis brevis and abductor pollicis longus.
It causes pain on the dorsal surface of the wrist at the radial side, sometimes extending into the base of the thumb.
It is typically causes by overuse, especially in those in whom there is a new and sudden increase in a specific repetitive activity (a.g. assembly line workers). It is also seen in racket sport players and golfers, and occasionally postpartum or in childcare workers (from repetitive lifting of children).
- Sometimes occurs after direct trauma to the 1st compartment
It is more common in women with a typical age of onset is 30-50. Symptoms may be bilateral.
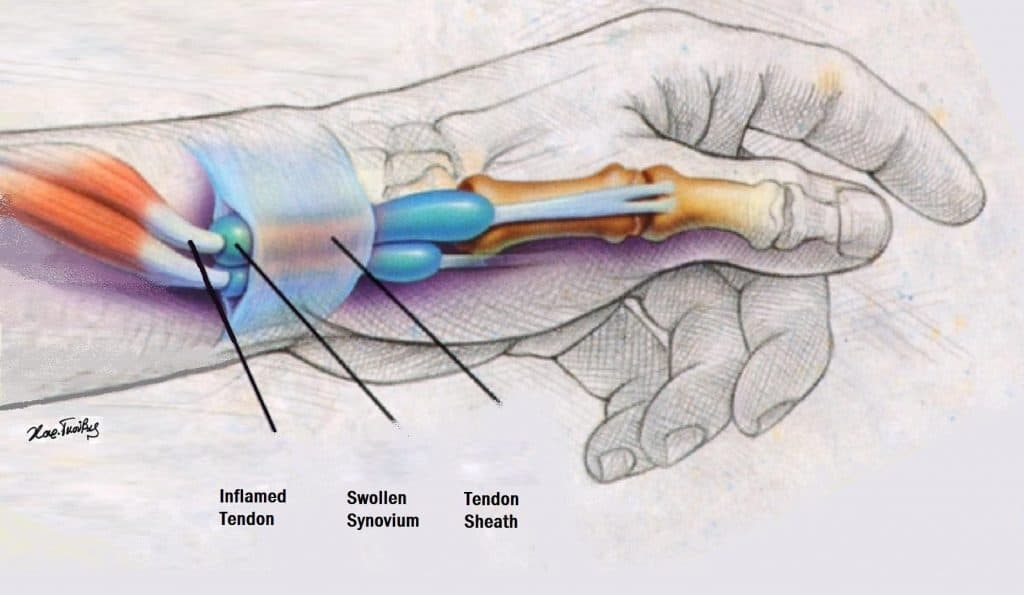
There is thickening and swelling of the extensor tendon retinaculum, which causes friction and pain. There is some debate as to whether or not it is truly an inflammatory condition.
Most cases resolve with non-operative management, but here is a high rate of recurrence.
Presentation
- Typically gradual onset
- Radial side wrist pain
- Tenderness +/- swelling / thickening over the area just proximal to the radial styloid
- Pain exacerbated by pinching and grasping objects, or by thumb or wrist movement
- Finkelstein manœuvre
- The thumb in placed in the palm, with the fingers folded over – to make a fist
- Wrist is adducted (toward the ulnar side)
- A positive test is where pain is felt in the radial side of the wrist during this adduction

Diagnosis is usually clinical. Occasionally x-ray may be performed to help rule out arthritis (e.g. osteoarthritis of the thumb).
Management
First line
- Rest
- Avoid provocation activities
- Wrist and thumb split
- Consider trial of NSAIDs for 2-3 weeks
- Consider referral to hand physiotherapist
Second line
- Consider in cases that have not settled after 4-6 weeks with conservative management
- Corticosteroid injection into the first dorsal compartment
- Technique
- Identify landmarks – including the radial artery, and the site of most tenderness
- Insert the needle about 1cm distal to the point of most tenderness
- Injected into the tendon sheath
- You should be able to palpate the tendon sheath expanding
Surgical
- Required in resistant cases
- Usually patient should have attempted at least 6 months of non-operative therapies without success
- The compartment is “released” – i.e. the tendon sheath is cut to prevent the friction occurring underneath it.
Differential Diagnosis
- Intersection syndrome – another painful MSK wrist disorder, in a similar location to De quern tenosynovitis
- In intersection syndrome, the tendons of the 1st compartment, rub up against the tendons of the second compartment, causing a bursitis
- Will usually have a negative Finkelstein test
References
- De Quervain’s tenosynovitis – orthobullets
- Murtagh’s General Practice. 6th Ed. (2015) John Murtagh, Jill Rosenblatt
- Oxford Handbook of General Practice. 3rd Ed. (2010) Simon, C., Everitt, H., van Drop, F.
- Beers, MH., Porter RS., Jones, TV., Kaplan JL., Berkwits, M. The Merck Manual of Diagnosis and Therapy




