
Contents
This article contains information about Novel Coronavirus (COVID-19) – which in March 2020 was declared a pandemic by the WHO. Information and public health advice about the virus (SARS CoV-2) and the illness it causes (COVID-19) is changing rapidly. It is recommended that you seek the advice of your local government health authority for the latest information.
Introduction
Coronaviruses are a family of viruses that cause respiratory infections in humans. Most coronaviruses cause a mild illness – for example – coronaviruses are responsible for about 1/4 of cases of the common cold.
However, some coronaviruses can cause severe respiratory distress, due to complications such as pneumonia and ARDS, and can have a significant mortality rate.
Significant outbreaks of deadly coronaviruses include:
- Middle East Respiratory Syndrome (MERS-CoV) – which caused various outbreaks in the 2010s. MERS had a mortality rate of about 35%
- Severe Acute Respiratory Syndrome (SARS-CoV) – which caused an outbreak in China and Hong Kong in 2002-03. SARS had a mortality rate of about 10%
- Novel coronavirus (SARS-CoV-2) which causes the illness known as COVID-19. Current estimates put the mortality rate at around 1-2% in unvaccinated individuals.
- The virus itself is officially called SARS CoV-2
- The illness it causes is known as COVID-19
- COrona VIrus Disease 2019
- The term COVID-19 is often used interchangeably for both purposes
- The term “novel” refers to the fact that it is a new strain – not previously identified in humans. Novel viruses often carry a worse prognosis, because the immune system has very little defence against these viruses because it has never encountered similar viruses
Novel coronavirus was first identified in the city of Wuhan in Hubei, China, around the end of 2019. It is believed to have originated in the live animal market in Wuhan – probably in bats (not as first suggested the pangolin). It was discovered after there were a cluster of unusual pneumonia cases within the city.
It mainly causes a respiratory disease.
By January 2020 it was confirmed to be spreading from person to person.
In March 2020 it was declared a pandemic by the WHO. Around the world in March and April 2020, countries imposed tight restrictions on movement of people, commonly referred to as “social distancing” in an attempt to reduce the spread of the disease.
Multiple vaccines were developed, and vaccination programmes began around the world in late 2019, and are ongoing.
There are also multiple treatments available for COVID-19, some of which are discussed below.
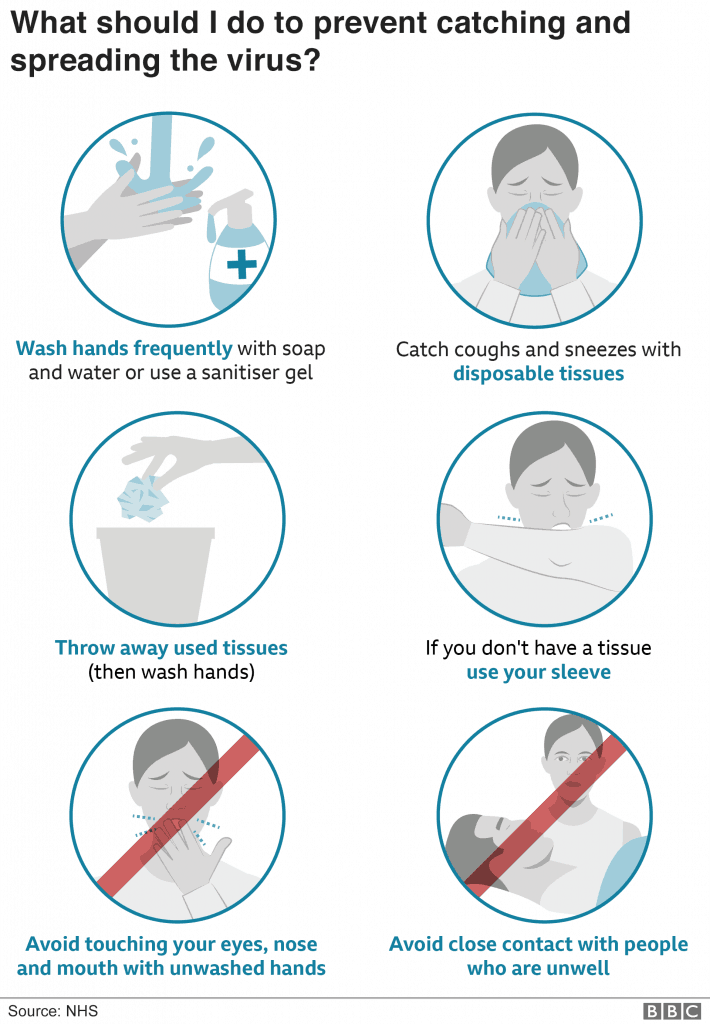
Stringent hygiene such as regular hand-washing and avoiding touching your face, and use of face masks can reduce the risk of infection. Public health measures to limit person to person contact may help to reduce the rate of spread amongst the population.
- It is highly likely that the vast majority of cases are from airborne transmission. Transmission from contaminated object (“fomites”) is now thought to be quite rare and may account only for about 1 in 1000 to 1 in 10 000 cases.
The virus seems to disproportionally affect older patients and those with pre-existing health conditions. Cases in children tend to be less severe.
It is expected that the CVOID-19 virus will become “endemic” – i.e. it will be present into the long-term, and may follow predictable patterns that cause larger outbreaks – like the flu.
Antibody levels to SARS-CoV-2 decline significantly over a period of months after infection and vaccination. The COVID-19 virus also mutates quickly (over periods of weeks to months) and as such re-infection is common.
Presentation
- Can be very variable
- An unknown proportion (estimates vary from 1 – 30%) are asymptomatic
- The illness peaks between days 9-13
- Most patients who become sick enough to require hospital admission have presented by day 5
- Typical presentations involve flu-like symptoms such as:
- Fever – 88%
- Cough – 67%
- Fatigue – 38%
- Shortness of breath – 18%
- Muscle aches – 15%
- Headache – 14%
- Sore throat – 14%
- Coryza – 5%
- Nausea / vomiting – 5%
- Diarrhoea – 4%
- Rarely there may also be:
- Meningitis
- Encephalitis – including agitation, confusion, altered consciousness
Symptom severity
- 80% of cases are mild and can be treated at home
- 20% of cases (in unvaccinated individuals) require hospital admission – typically for treatment of shortness of breath secondary to pneumonia or ARDS
- 5% of cases (in unvaccinated individuals) require ICU admission – typically for ARDS, respiratory failure, sepsis and multi-organ failure
- The median time from onset to ICU admission is 10 days
- Average time from symptom onset to death is 2-8 weeks
Phenotypes
Some Emergency Medicine and ICU specialists in hard-hit countries (particularly the USA) are starting to talk in-terms of three types of presentation:
- Mild flu-like illness
- These patients do not have respiratory distress, and typically present with mild flu-like symptoms
- These patients can be safely managed at home
- “Happy hypoxic”
- These patients present with low O2 sats (typically in the 70-80% range), but otherwise appear well
- They typically do NOT have tachycardia or increased respiratory rate or increased work of breathing. Their blood-pressure is usually normal
- The patients should be admitted to hospital for basic oxygen therapy
- Advising these patients to sit up (out of bed in a chair, or in bed) or to lie ‘prone’ (lie on their front) can help to improve the hypoxia
- Despite the very low O2 saturations, it doesn’t appear to be beneficial to intubate or ventilate these patients
- More severe patients may be considered for NIV (CPAP)
- Severely unwell patient
- These patients often have extremely low oxygen saturations – numbers that may initially seem incompatible with life – such as 25-40%
- Their other vital signs may also suggest a severely unwell patient – such as tachycardia and hypotension
- They will require intubation and ventilation and ICU admission
- CPAP may be used as a temporary measure to assist with pre-oxygenation before intubation
Infectivity
The Ro number refers to on average how many people and affected person will infect.
- A disease with an Ro on <1 will typically slowly decline in number of cases, and eventually disappear
- A disease with an Ro number of >1 can propagate widely throughout a population
- The Ro of coronavirus is estimated to be 1.5 – 3.4
- Ro of influenza is about 1.3
For a really interesting interactive simulation on infectivity, and how it can be altered using social isolation methods, try this simulation from The Washington Post.
Incubation
- The average incubation period is 5 days
- The typical range is between 2-14 days
- There is a single confirmed case after 27 days incubation
- 75% show symptoms before 7 days
- <1% show symptoms after 14 days
- It is believed that the virus can be shed during the asymptomatic incubation period, or in individuals who are completely asymptomatic
Transmission
- Transmission occurs from person to person by droplet transmission, mucous membranes, faecal-oral route and via fomites (contaminated inanimate objects – such as door handles and other surfaces)
- The virus can survive for up to 4 days on surfaces (duration of survival depends on the surface – plastic and wood surfaces have longer duration of survival than metal). It is not clear if it retains the ability to be infective for this period.
- Respiratory droplets (>5um) are the major form of transmission
- These are produces by coughing, sneezing and breathing
- Respiratory droplets typically stay in the air for <17 minutes, and only travel about 1m. Sneezing and aerosolising procedures can transmit droplets further than 1m.
- Respiratory droplets land on inanimate objects – such as surfaces, clothes etc. These are known as fomites.
- Infection can occur when an uninfected individual touches a “fomite” and then subsequently transfers the droplets to a mucous membrane – e.g. the eye, mouth or nose.
- “Aerosolising” procedures are medical procedures thought to increase the spread of smaller aerosol droplets (<5um). These include the use of nebulizers, bag-valve-mask ventilation, and non-invasive ventilation (e.g. CPAP).
- It is not yet proven that this can lead to transmission of SARS-CoV2
Pathogenesis
- Coronaviruses have transmembrane glycoproteins – known as “spike proteins” on their surface, that attach to the target cells
- It appears that SARS-CoV2 attaches to Angiotensin converting enzyme 2 (ACE2) receptors
- ACE2 is expressed in the lungs and upper respiratory tract cells, and to a lesser extent, in the small intestine
- Once inside the cell, viral RNA replication occurs
- In patients who develop severe life-threatening illness it is believed that an extreme immune response (Sometimes referred to as a “cytokine storm“) may be responsible for many of the effects, rather than a direct effect of the virus itself
- This can lead to ARDS, SIRS, and heart failure, as well as other end-organ failure
There has been some speculation as to the role of ACE-inhibitors and angiotensin receptor blockers in the treatment of COVID-19. At the moment it remains just that – speculation. Initially there were some fears that these medications were associated with a worse prognosis, but more recently, there are suggestions that they may improve prognosis. Know one really knows at present, but there is no official advice to cease these medications in patients suffering from or at high risk of COVID-19.

Diagnosis
Diagnosis is typically confirmed by a PCR swab of the nasopharynx and oropharynx. Some jurisdictions recommend using the same swab in both locations. Depending on the lab, PCR testing can take anywhere from 6 hours to several days. Check your local testing guidelines. Initial restrictions to testing due to lack of capacity have mostly now been relaxed and in most countries and jurisdictions testing is available to anybody with URTI symptoms.
Respiratory PCR
- Between 60-85% senstivie
- i.e. between 15-40% of truly infected patients will be false negatives
Rapid antigen test (RAT)
- Easy-to-use kits that can be done at home by patients
- Results in 10-20 minutes
- Less accurate than PCR – sensitivity and specificity vary by brand and testing technique (often poor when done at home by unsupervised patients!)
- The best tests are believed to be about 70% sensitive, with high specificity (low false positive rate)
I advise my patients that a positive RAT indicates that they definitively have COVID-19. A negative test, in the presence of symptoms does NOT rule out COVID-19 and these patients should consider PCR testing (depending on local jurisdiction guidelines) – Dr Tom Leach
Other testing methods
- Viral culture is not recommended for safety of lab technicians
Serology
- A serology (blood / serum) test is available
- This can detect the presence of antibodies (Ig) to coronavirus
- This test typically becomes positive within several weeks of contracting the infection and likely remains positive for months or even years after the infection
- In theory, these test can give a result in 15 minutes
- Generally this testing is used only in population level studies to assess the previous exposure to coronavirus. It is often not able to reliably detect current infection, and is mainly useful to show past infection
- As of June 2022 it is believed that >90% of individuals in the UK have had COVID-19
Consider COVID-19 in any patient with:
- Cough, OR
- Fever, OR
- Any other respiratory or upper respiratory tract symptoms
- There is no way to reliably distinguish COVID-19 from other respiratory virus infections clinically
Other investigations
Blood tests
- FBC – lymphocytopaenia
- About 45% of patients
- 85% of critically ill patients
- WCC can be normal, high or low
- Coagulation studies
- Usually normal except in DIC (a life-threatening complication of SIRS)
- U+Es – usually normal
- LFTs
- ALT / AST / bilirubin – may be increased
- 40-75% of cases
- >90% of ICU cases
- Might be useful as a marker of severity
- Inflammatory markers
- CRP – increased
- ESR – increased
- Albumin – decreased
- Ferritin – increased
- Lumbar puncture – consider if signs of meningitis
- Others
- Troponin and D-dimer are often increased
Imaging
The findings in COVID-19 are no different to other causes of a viral pneumonia – there are no specific COVID-19 imaging changes. The typical finding is bilateral opacities. These may start as unilateral and later progress to bilateral. The changes typically evolve over 1-3 weeks and usually peak at around 10-12 days.
X-ray and CT changes may also be visible in asymptomatic individuals.
The amount of lung involved is proportional to the severity of the disease.
Chest X-ray
- Bilateral opacities
- Rarely – pleural effusions
CT chest
- Bilateral ground glass infiltrates
- Seen in >80% of cases
- Not specific, but can be considered diagnostic in the context of clinical symptoms consistent with coronavirus
Ultrasound
- May be useful as a bedside test in the emergency setting
- Again – changes are the same as those seen in all viral pneumonias – and not specific to COVID-19
- “B-lines”
- Irregular pleural line
Complications
- Encephalitis
- Guillain-Barre Syndrome
- Myocarditis
- Cardiomyopathy
- Acute kidney injury
- Acute liver injury
- Rhabdomyolysis
- Co-infection with other pathogens
- Multi-organ failure
- DIC
- SIRS
Management
Guidelines for the management of COVID-19 can be pretty complicated!
As of July 2022, generically it is recommend that any patient with a sensation of SOB be treated with an inhaled corticosteroid.
There are many anti-virals and other treatments available with various qualifying criteria. For example, those over 65 with other risk factors (such as hypertension, obesity, known cardiovascular disease) should be offered Paxlovid in Australia.
There are various other drugs offered to those who are unvaccinated or immunocompromised based on the severity of their disease.
In addition, the following supportive treatments are used:
Mild infection
Mild cases can be managed safely at home. Advise should be similar to that of other common upper respiratory tract infections, such as:
- Simple analgesia – e.g. paracetamol 1g QID
- Oral fluids – titrate to urine output – aim for straw coloured urine, passing urine at least x3 per day
- Safety-net instructions – such as – advise to seek medical review if increasing shortness of breath, light-headed or dizzy (pre-syncope), or syncopal symptoms, or generally unwell
Self isolation is an important public health measure for anybody with confirmed or suspected COVID-19.
- Self isolation should last until symptoms have resolved, OR
- Self-isolation should involve:
- Staying at home, or your hotel or place of residence
- Going outside to private gardens is OK
- NOT allowing visitors
- DO NOT visit public places, including schools, work, childcare, university, other public gatherings
- DO NOT use public transport
- Ask friends or relatives who are not in isolation to fetch food and any other items you many need. Online shopping may also be an option
- Infected patient should wear a face mask in any communal areas of the home to reduce the risk of droplet transmission
- Other people in the house:
- Will also be required to self-isolate if they have been in close contact with a confirmed infection (see close contact rules, above)
- Coping with self isolation
- Keep a regular routine – e.g. eating regular meals
- Work from home if possible
- Take regular exercise
- Arrange activities for children – and try to keep up with any school-work via email or other electronic means
- Staying at home, or your hotel or place of residence
- Cleaning around the house to minimise transmission – regular household detergent is suitable. Advise patients to regular wash any surfaces that are frequently touched in the home, such as:
- Door handles
- Light switches
- Kitchen and bathroom areas
Indicators of mild infection include:
- No shortness of breath
- O2 sats >92% on room air
- Speaking in full sentences
- Respiratory rate not raised
- No signs of increased work of breathing
- Not hypotensive
- No symptoms of pre-syncope or syncope, or signs of postural hypotension
- Normal heart rate – not tachycardic (HR <100)
Severe infection
- About 20% of cases in unvaccinated individuals require hospital admission
- The mainstay of treatment is supportive respiratory care – such as:
- Oxygen to maintain O2 sats >= 93%
- Intubation and ventilation in the most severe cases
- Other organ support in multi-organ failure
- Typical time from onset of illness to development of ARDS is 8-9 days
- 10% of patients develop secondary infections
Oxygenation
Aim for the usual oxygenation targets:
- Sats >92% for most patients
- Sats 88-92% for patients with known COPD with CO2 retention
Types of oxygen supply device that can be safely used with standard droplet precautions:
- Nasal prongs / cannulae
- Hudson mask
- Non-rebreather mask
- Venturi mask
In patients who still do not maintain adequate oxygenation, despite these measures then forms of assisted ventilation – such as non-invasive ventilation (NIV) and intubation should be considered.
NIV devices are somewhat contentious. In theory they can produce aerosolised particles, and some studies of the SARS outbreak showed an increased risk of healthcare worker transmission when they were used. NIV devices included high-flow nasal cannulae (HFNC) and CPAP / BiPAP type devices with face masks (of various types).
Current recommendations generally suggest that:
- HFNC are recommended for use in acutely hypoxic patients
- Consider airborne and contact precautions
- Other types of NIV should be used with caution in COVID-19, and with airborne precautions
- A suggested approach is to use other forms of NIV only as a pre-oxygenation device when preparing for intubation
Intubation
- Early experience in China led to a high rate of intubations – mainly based on the typical parameters used for intubation based on oxygenation
- However, subsequent experience in Europe and the USA has suggested that many patients with low oxygenation who are otherwise not distressed (the “happy hypoxics” described above) may have a better outcome by avoiding intubation
- As such, it may now be advisable for those even with poor oxygenation, if they are alert, do NOT have tachycardia or hypotension, and are able to “prone” themselves (lie on their front) – that they should not be intubated, and instead can tolerate low O2 sats whilst ever they still meet the parameters above
- The intubation procedure itself presents a very high level of risk to the staff involved
- High levels of PPE are recommended
- Avoid bag-valve-mask ventilation (BVM)
- Use video laryngoscope
- Avoid auscultating the chest after intubation
- Use viral filters on ventilators
- Consider taping all connections in the ventilator tubing – disconnections could be spraying the virus around the room
- Advice for ventilation
- Similar to ARDS management
- Tidal volume of 4-6 mL/Kg
- Plateau pressures <30 cmH20
- Allow hypercapnia as long as pH maintained >7.15
- Consider prone positioning if oxygenation is insufficient
Complications
- The long term effects are still unclear
- Reports include:
- Cardiac complications
- Respiratory complications – particularly pulmonary fibrosis
- Stroke
- Other chronic neurological complications
Prevention
Basic hygiene measures may help to reduce the spread of the virus. Face mask wearing is now thought to be particularly important in reducing the spread of the virus.
Prognosis
In unvaccinated patients:
- 80% of patients have mild symptoms – similar to a common cold or the flu
- 20% of patients require hospital admission
- 5% require ICU admission
- Novel coronavirus has about a 2% mortality
- This is not evenly distributed, and disproportionally affects older and co-morbid populations
- The exact mortality rate cannot be accurately calculated until after the outbreak is over – through retrospective testing of the population for coronavirus antibodies to calculate the true incidence of the disease
Mortality by age
Most sources suggest that men are more likely to die than women, but this is not yet proven.
Age | Mortality rate |
| 80+ | 15% |
| 70-79 | 8% |
| 60-69 | 3.6% |
| 50-59 | 1.3% |
| 40-49 | 0.4% |
| 30-39 | 0.2% |
| 20-29 | 0.2% |
| 10-19 | 0.2% |
| 0-9 | <0.1% |

Mortality by pre-existing condition
Pre-existing condition | Mortality rate |
| Cardiovascular disease | 10% |
| Diabetes | 7% |
| Chronic Respiratory disease | 6% |
| Hypertension | 6% |
| Cancer | 6% |
| None | 0.9% |

Public health implications
- Peak incidence in any given country or region is expected to occur about 2 months after the first cases
- 20-80% of the population is likely to be infected
- Duration of the pandemic is likely to be 6-12 months
- After this, the future of the virus is uncertain. It may become endemic – circulating amongst the population indefinitely.
- This could be either as a seasonal illness and rapidly mutating illness – like influenza – or as a non-seasonal disease – like chicken-pox
- A vaccine is under development but will probably not be available until late 2020 at the earliest
- Previous infection is likely to provide immunity for at least several years – but this is not known for sure
- The aim of public health measures is to slow the rate of spread
References
- Coronavirus disease 2019 (covid-19): a guide for UK GPs
- WHO – Coronavirus disease (COVID-19) outbreak
- Clinical care – Coronavirus Disease 2019 (COVID-19) – CDC
- Coronavirus cases – Worldometer
- COVID-19 Data pack – information is beautiful
- Coronavirus disease (COVID-19) – Isolation guidance – health.gov.au
Real estimates of mortality following COVID-19 infection – The Lancet
- Coronavirus disease 2019 (COVID-19) – LIFTL
- A practical COVID-19 resource for Emergency Medicine – Emergency Medicine Cases





Pingback: I can’t burp | almostadoctor
I thought dexamethazone can improve symptoms , why steroids are contraindicated ?
Hi Husein – thanks for spotting this – the recommendation to avoid corticosteroids is now outdated. However, despite many major news outlet reporting the “breakthrough” of dexamethasone usage a few weeks ago, I have not found any guidelines which as of yet recommend its routine use.