
Contents
Haemorrhoids
Haemorrhoids are a swelling and inflammation of the veins in the rectum and anus. They are THE most common cause of rectal bleeding. They are extremely common in adults.
Aetiology
- Associated with constipation (it is thought haemorrhoids can develop as a result of straining)
- Often develop for the first time during pregnancy.
- Caused by congestion of the internal and/or external venous plexuses in the anal region.
Clinical Features
- Bleeding – the blood will be bright red
- Discomfort
- May become thrombosed (a blood clot forms inside the haemorrhoid), in which case they often become inflamed and very painful
- Pruritus ani – this is irritation of the skin around the anus, and usually causes the desire to scratch. It has many causes.
- Mucus discharge
- They may produce blood on the toilet paper and blood on the outside of the stools.
- Pain on passing stool (external haemorrhoids only)
Pathology
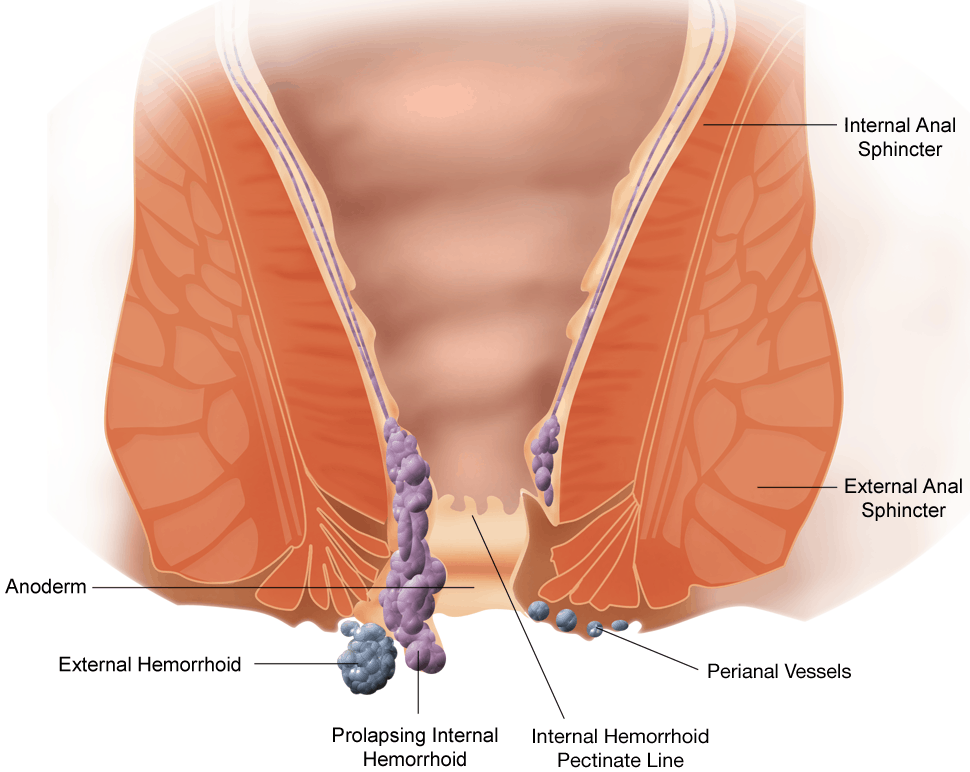
Internal haemorrhoids
Are typically painless, and covered with music. As they arise internally, there are no pain receptors in this area, hence them being painless.
- Primary (internal) – these may cause bleeding, but are not visible from the outside
- Second degree (prolapsing) – these can also bleed, and may ‘pop out’, but they can retract (and prolapse again) spontaneously.
- Third degree (prolapsed) – these require manual replacement after they have prolapsed.
- Foruth degree – prolapsed and cannot be replaced
External haemorrhoids
Painful, and typically covered with skin.
- Form at the anal opening
- Especially painful if they develop thrombosis (at which point they will be firm and exquisitely tender!)
- If thrombosis occurs it typically resolves over a period of weeks, and the haemorrhoid will shrink down and size and then generally be less troublesome. May thrombus and flare-up again
Treatment
Primarily involves measures to prevent constipation and straining, as well as topical creams that may relieve acute symptoms.
- Stool softeners – such as movicol or other bulk-forming laxatives
- Also ensure a high fibre diet, and adequate fluid intake
- These help to prevent thrombosis of haemorrhoids
- Topical agents
- Anusol – zinc oxide with balsum peru. Provides some topical analgesia
- Proctosedyl – contains hydrocortisone and cinchocaine (a local anaesthetic). Provides topical symptomatic relief
- 2% diltiazem cream – diltiazem is a calcium channel blocker most commonly taken orally as an anti-hypertensive or for its cardiac effects. It is also used topically for anal fissure, and occasionally for haemorrhoids to. It may help to reduce the size of the haemorrhoids. Thought to reduce anal sphincter tone, which in turn increases blood flow and promotes healing.
The only definitive treatment is to have the haemorrhoid removed. This requires more invasive techniques, which may include:
- Sclerotherapy – this involves an injection into a vein that causes it to dramatically shrink. It can also be used on lymphatic drainage vessels. It is a common procedure to treat haemorrhoids and varicose veins in adults. The vein is injected with a sclerosing agent, which will make the vein immediately shrink. Over the next few weeks, the vein tissue will be absorbed by the body.
- This is particularly effective for treating vein problems because it also helps to sclerose feeder veins, and this prevents recurrence of the problem. It is often the preferred treatment for small varicose veins and haemorrhoids.
- Band ligation – a small band is tied round the vessel and this restricts the blood flow, and the vessel will be absorbed (as seen in treatment of oesophageal varices).
- Haemorrhoidectomy is also sometimes performed. This is usually curative. The vein is surgically removed.
Anal Fissures
- An anal fissure is a tear in the skin that lines the anus below the level of the dentate line. It will be painful on defecation.
- It can be a primary problem in young to middle-aged adults, but also is associated with Crohn’s and UC.
- They most commonly occur in the midline posteriorly.
- An oedemomatous skin tag is common next to the lesion. This is sometimes called a sentinel pile.
- The fissures can often be seen externally, but examination is difficult due to pain and sphincter spasm. Sphincter spasm may also impair wound healing.
- Treatment usually involves an anaesthetic cream and a stool softener.
- Nitric oxide (GTN cream) may also be given to aid relaxation of the internal sphincter.
- 2% diltiazem cream is also used. Thought to reduce anal sphincter tone, which in turn increases blood flow and promotes healing.
Fistula in ano
- These most commonly result from infection of anal glands by normal colonic bacteria. They also occur in Crohn’s disease.
- They usually present as abscesses and heal once the abscess is excised.
- Management is usually surgical – 90% of fistulas are managed in this way.
Anorectal abscesses
- Anorectal abscess are 3x as common in men as women
- They are more common in people engage in penetrative anal sex, including men who have sex with men (MSM)
- Anorectal abscesses are a common cause of admission to hospital.
- They are often the first manifestation of Crohn’s, UC and TB.
- They will present with painful tender swellings and discharge.
- They are surgically excised and drained, and follow up treatment is with antibiotics. Before this takes place they are sometimes imaged with MRI, perhaps also with local anaesthetic and ultrasound.
Rectal prolapse, intussusception and solitary rectal ulcer syndrome (SRUS)
- All these conditions are thought to be interrelated, with the underlying cause thought most commonly to be rectal prolapse.
- Rectal prolapse is basically where the walls of the rectum will protrude through the opening of anus and become visible. Normally, rectal prolapse starts out as an intussusception – this is where part of the intestine slides into another part, in the way parts of a telescope slide into eachother. Gradually this intussusception gets bigger and bigger until eventually, it prolapses out of the anus. Constipation and chronic straining are a likely cause. However, in addition to this, the presence of an intussusception in the rectum will lead to a feeling of a stool in the rectum (tenesmus), and will mean that the patient will feel the need to defecate.
- In some patients, repeated straining will lead to the formation of a SRUS, usually on the anterior wall of the rectum. SRUS is not as simple as it sounds. It causes local inflammatory changes that appear non-specific on histological examination. It may also be difficult to distinguish from cancer on endoscopic examination.
- Patients usually present with slight bleeding and the presence of mucus on defecation. There may also be tenesmus and a feeling of incomplete defecation.
- Asymptomatic SRUS should not be treated. Otherwise, patients should be advised not to strain, and should take stool softeners.
- If rectal prolapse can be demonstrated on defecation, then this may need to be treated surgically.
References
- Murtagh’s General Practice. 6th Ed. (2015) John Murtagh, Jill Rosenblatt
- Oxford Handbook of General Practice. 3rd Ed. (2010) Simon, C., Everitt, H., van Drop, F.
- Beers, MH., Porter RS., Jones, TV., Kaplan JL., Berkwits, M. The Merck Manual of Diagnosis and Therapy




